PEAK FLOW METER?
A Peak Flow Meter is a portable, inexpensive, hand-held device used to measure how air flows from your lungs in one "fast blast." In other words, the Meter measures your ability to push air out of your lungs.
Peak Flow Meters may be provided in two ranges to measure the air pushed out of your lungs. A low range Peak Flow Meter is for small children, and a standard range meter is for older children, teenagers and adults. An adult has much larger airways than a child and needs the larger range.
There are several types of Peak Flow Meters available. Talk to your doctor or pharmacist about which type to use.
WHO CAN BENEFIT FROM USING A PEAK FLOW METER?
Many doctors believe that people who have asthma can benefit from the use of a Peak Flow Meter. If you need to adjust your daily medication for asthma, a Peak Flow Meter can be an important part of your asthma management plan.
Children as young as three years have been able to use a Meter to help manage their asthma. In addition, some people with chronic bronchitis and emphysema may also benefit from the use of a Peak Flow Meter.
Not all physicians use Peak Flow Meters in their management of children and adults with asthma. Many doctors believe a Peak Flow Meter may be of most help for people with moderate and severe asthma. If your asthma is mild or you do not use daily medication, a Peak Flow Meter may not be useful for asthma management.
WHY SHOULD I MEASURE MY PEAK FLOW RATE?
Measurements with a Peak Flow Meter can help you and your doctor monitor your asthma. These measurements can be important and help your doctor prescribe medicines to keep your asthma in control.
A Peak Flow Meter can show you that you may need to change the way you are using your medicines. For example, Peak Flow readings may help be a signal for you to implement the medication plan you and your doctor have developed for worsening asthma.
On the other hand, if you are doing well, then measuring your Peak Flow may be helpful as you and your doctor try to lower the level of your medicines.
A Peak Flow Meter can help you when your asthma is getting worse. Asthma sometimes changes gradually. Your Peak Flow may show changes before you feel them. It can allow your doctor to adjust your treatment to prevent urgent calls to the doctor, emergency room visits or hospitalizations.
A Peak Flow Meter may help you and your doctor identify causes of your asthma at work, home or play. It may help parents to determine what might be triggering their child's asthma.
A Peak Flow Meter can also be used during an asthma episode. It can help you determine the severity of the episode; decide when to use your rescue medication; and decide when to seek emergency care.
Knowing your "personal" Peak Flow Rate allows you to elevate your readings. Being at your "best" can provide reassurance and make you feel more self-confident.
HOW DO YOU USE A PEAK FLOW METER?
Step 1: Before each use, make sure the sliding marker or arrow on the Peak Flow Meter is at the bottom of the numbered scale (zero or the lowest number on the scale).
Step 2: Stand up straight. Remove gum or any food from your mouth. Take a deep breath (as deep as you can). Put the mouthpiece of the Peak Flow Meter into your mouth. Close your lips tightly around the mouthpiece. Be sure to keep your tongue away from the mouthpiece. In one breath blow out as hard and as quickly as possible. Blow a "fast hard blast" rather than "slowly blowing" until you have emptied out nearly all of the air from your lungs.
Step 3: The force of the air coming out of your lungs causes the marker to move along the numbered scale. Note the number on a piece of paper.
Step 4: Repeat the entire routine three times. (You know you have done the routine correctly when the numbers from all three tries are very close together.)
Step 5: Record the highest of the three ratings. Do not calculate an average. This is very important.
You can't breathe out too much when using your Peak Flow Meter but you can breathe out too little. Record your highest reading.
Step 6: Measure your Peak Flow Rate close to the same time each day. You and your doctor can determine the best times. One suggestion is to measure your Peak Flow Rate twice daily between 7and 9 a.m. and between 6 and 8 p.m.
You may want to measure your Peak Flow Rate before or after using your medicine. Some people measure Peak Flow both before and after taking medication. Try to do it the same way each time.
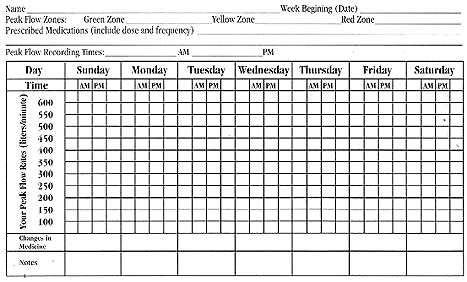
Step 7: Keep a chart of your Peak Flow Rates. Discuss the readings with your doctor.
HOW DO I CHART MY PEAK FLOW RATES?
Chart the HIGHEST of the three readings. The chart could include the date at the top of the page with AM and PM listed. The left margin could list a scale, starting with zero (0) liters per minute (L/min) at the bottom of the page and ending with 600 L/min at the top.
You could leave room at the bottom of the page for notes to describe how you are feeling or to list any other thoughts you may have.
WHAT IS A "NORMAL" PEAK FLOW RATE?
A "normal" Peak Flow Rate is based on a person's age, height, sex and race. A standardized "normal" may be obtained from a chart comparing the patient with a population without breathing problems.
A personal best normal may be obtained from measuring the patient's own Peak Flow Rate. Therefore, it is important for you and your doctor to discuss what is considered "normal" for you.
Once you have learned your usual and expected Peak Flow Rate, you will be able to better recognize changes or trends.
HOW CAN I DETERMINE A "NORMAL" PEAK FLOW RATE FOR ME?
Three zones of measurement are commonly used to interpret Peak Flow Rates. It is easy to relate the three zones to the traffic light colors: green, yellow, and red. In general, a normal Peak Flow Rate can vary as much as 20 percent.
Be aware of the following general guidelines. Keep in mind that recognizing changes from "normal" is important. Your doctor may suggest other zones to follow.
Green Zone:
80 to 100 percent of your usual or "normal" Peak Flow Rate signals all clear. A reading in this zone means that your asthma is under reasonably good control. It would be advisable to continue your prescribed program of management.
Yellow Zone:
50 to 80 percent of your usual or "normal" Peak Flow Rate signals caution. It is a time for decisions. Your airways are narrowing and may require extra treatment. Your symptoms can get better or worse depending on what you do, or how and when you use your prescribed medication. You and your doctor should have a plan for yellow zone readings.
Red Zone:
Less than 50 percent of your usual or "normal" Peak Flow Rate signals a Medical Alert. Immediate decisions and actions need to be taken. Severe airway narrowing may be occurring. Take your rescue medications right away. Contact your doctor now and follow the plan he has given you for red zone readings.
Some doctors may suggest zones with a smaller range such as 90 to 100 percent. Always follow your doctor's suggestions about your Peak Flow Rate.
MANAGEMENT PLAN BASED ON PEAK FLOW READINGS
It is important to know your Peak Flow reading, but it is even more important to know what you will do based upon that reading. Work with your doctor to develop an asthma management plan that follows your green-yellow-red zone guidelines.
Record the Peak Flow readings that your doctor recommends for your green zone, yellow zone, and red zone. Then work out with your doctor what you plan to do when your Peak Flow falls in each of those zones.
WHEN SHOULD I USE MY PEAK FLOW METER?
Use of the Peak Flow Meter depends on a number of things. Its use should be discussed with your doctor.
If your asthma is well controlled and you know the "normal" rate for you, you may decide to measure your Peak Flow Rate only when you sense that your asthma is getting worse. More severe asthma may require several measurements daily - or twice a day.
Don't forget that your Peak Flow Meter needs care and cleaning. Dirt collected in the meter may make your Peak Flow measurements inaccurate. If you have a cold or other respiratory infection, germs or mucus may also collect in the meter.
Proper cleaning with mild detergent in hot water will keep your Peak Flow Meter working accurately and may keep you healthier.
DOES USING A PEAK FLOW METER HAVE ANY SIDE EFFECTS?
A Peak Flow Meter is not a medicine. It has no major side effects. Sometimes pushing the air out of your lungs in a "fast blast" may cause you to cough or wheeze.
Check with your doctor before you start using a Peak Flow Meter.
Using the meter is as simple as taking a deep breath and blowing out a candle. If used properly, it can only help.
You must realize that measuring Peak Flow is only one step in a program to manage asthma. Its importance must not be exaggerated or over-interpreted.
Using a Peak Flow Meter is not a substitute for regular medical care. Ask your doctor to help you understand your Peak Flow measurements.
IDEAS TO REVIEW
Now you are aware of some of the techniques for using and caring for Peak Flow Meters. You also know how Meters may help manage asthma and other breathing problems.
Discuss the use of a Peak Flow Meter with your doctor. Make measuring your Peak Flow Rate a part of your personal asthma management program.
The mission of the American Lung Association is to prevent lung disease and promote lung health.